David T. Turdy
What is ankylosing spondylitis (AS)?
In the early stages, ankylosing spondylitis and the related conditions are likely to cause:
- stiffness and pain in the lower back in the early morning which eases through the day or with exercise
- pain in the sacroiliac joints (the joints where the base of your spine meets your pelvis), in the buttocks or the backs of your thighs.
Some people first notice problems after a muscle strain, so the condition is often mistaken for common backache. However, stiffness that lasts at least 30 minutes in the morning helps to distinguish ankylosing spondylitis from simple back pain. The symptoms may also occur after rest, or may wake you in the night.
You may also have neck, shoulder, hip or thigh pain, which is often worse if you’ve been inactive for a time, for example if you work at a computer. Some people have pain, stiffness and swelling in their knees or ankles. In psoriatic arthritis, the smaller joints of the hands and feet may be affected. For some people, especially children and teenagers, the first signs may be in their hip or knee rather than their back.
Inflammation can occur anywhere in the body where tendons attach to bone (this is called enthesitis), for example, at the elbow and heel. Inflammation comes and goes so the symptoms may vary over time.
The inflammation that causes these symptoms comes and goes, so the degree of pain can vary over time and from person to person. If the condition is mild and only affects the sacroiliac joints, it may go almost unnoticed, but if most of the spine is affected it can cause difficulty with activities that involve bending, twisting or turning.
Other possible symptoms include:
- tenderness at the heel – This makes it uncomfortable to stand on a hard floor. Inflammation can occur at the back of your heel where the Achilles tendon meets the heel bone, or in the tendon in the arch of the foot which is known as plantar fasciitis.
- pain and swelling in a finger or toe – When the whole digit is swollen it’s known as dactylitis.
- tenderness at the base of your pelvis (ischium) – This makes sitting uncomfortable.
- chest pain or a ‘strapped-in’ feeling that comes on gradually – If your spine is affected at chest level (the thoracic spine) it can affect movement at the joints between the ribs and the breastbone, which makes it difficult for you to take a deep breath. Your ribs may be very tender, and you may feel short of breath after even gentle activity. Coughing or sneezing may cause discomfort or pain.
- inflammation of the eye (uveitis or iritis) – The first signs of this are usually a red (bloodshot), watery and painful eye, and it may become uncomfortable to look at bright lights. If this happens, or if you develop blurred vision, it’s important to get medical help within 24–48 hours. The best place to go is an eye casualty department – this might not be at your local hospital. Your GP surgery, local A+E or your optician will know where the nearest eye casualty department is. Treatment is usually with steroid eye drops, which are generally very effective. Some people get repeated attacks of eye inflammation, but they’re extremely unlikely to cause permanent damage if they’re treated promptly.
- inflammation of the bowel – People with ankylosing spondylitis can develop bowel problems known as inflammatory bowel disease (IBD) or colitis. Tell your doctor if you have diarrhoea for more than 2 weeks or begin to pass bloody or slimy stools. You might be referred to a bowel specialist (gastroenterologist). Symptoms of IBD can vary, but it can usually be treated successfully with medication. Sometimes treatments like non-steroidal anti-inflammatory drugs (NSAIDs) can make bowel problems worse, so you might be advised to stop taking them.
- tiredness – This may be caused by the activity of the condition, anaemia or sometimes depression and frustration associated with the condition.
Who gets ankylosing spondylitis (AS)?
Ankylosing spondylitis can affect anyone, although it’s most common in young men and most likely to start in your late teens or 20s.
The genes you inherit from your parents may make you more likely to develop AS, but the condition isn’t passed on directly. Most people with ankylosing spondylitis have a gene called HLA-B27, which can be detected by a blood test. This gene isn’t the cause of ankylosing spondylitis but it does contribute to it.
Having this gene doesn’t mean you’ll definitely get AS, and the blood test isn’t very useful in diagnosing the condition. Even in families where somebody’s been diagnosed with ankylosing spondylitis there may be brothers or sisters who have the HLA-B27 gene but who don’t have the condition.
What is the outlook for
ankylosing spondylitis (AS)?
Ankylosing spondylitis (AS) and the related conditions are quite variable and difficult to predict. They can cause a lot of pain, although treatment will help to ease this. You may have times when the symptoms become worse and other times when you find it easier to cope with the pain and stiffness. AS can make you feel generally unwell, lose weight or tire easily.
Most people with a spondyloarthritis have some stiffening in the spine, usually in the lower back. This can be painless and may not interfere with physical activity because the neck, hips, limbs and the upper part of your spine can remain quite mobile. However, if more of your spine stiffens or your knees or hips are affected, you may have more difficulty with mobility. Treatment can help prevent these mobility problems.
Very rarely, there may be complications affecting the heart, lungs and nervous system. The valves in the heart may leak, which can put it under more strain. And long-term inflammation and tissue scarring in the lungs can reduce rib movement, which means you can’t take in a full breath. Very rarely, the top of the lungs may become scarred. Fewer than 1 in 100 people with ankylosing spondylitis have these problems, and they are even less common in other types of spondyloarthritis. Even so, if you smoke, it’s extremely important to try to stop because smoking is likely to add to any heart or lung problems.
People with ankylosing spondylitis, especially those who’ve had the condition for a long time and whose vertebrae have fused, are at increased risk of spinal fractures following a trauma (for example, a fall or car accident). Spinal fractures can cause nerve damage, so it’s important to tell any doctor treating you following trauma that you have ankylosing spondylitis, especially if you have new unexplained pain in your spine or new weakness or tingling in your arms or legs. The fracture may not show easily on x-rays, so you may need a magnetic resonance imaging (MRI) or computed tomography (CT) scan.
Some people with ankylosing spondylitis develop osteoporosis (thinning of the bones), and it’s important that this is treated. Your doctor may suggest you have a bone density (DEXA) scan to check for this.
How is ankylosing spondylitis (AS) diagnosed?
Most back pain isn’t caused by ankylosing spondylitis (AS). However, the symptoms, especially in the early stages, can be very similar to more common back problems. Because of this, many people put up with the pain for some time before seeking help. When you first see your doctor, there may be little to show whether the problem is ankylosing spondylitis or some other, more common, back problem. Unfortunately, ankylosing spondylitis may even be misdiagnosed at first. Ankylosing spondylitis is normally diagnosed by a rheumatologist.
There’s no specific test that will confirm you have ankylosing spondylitis, so diagnosis involves piecing together information from different sources, including:
- the history of your condition (including whether pain and discomfort is waking you during the second half of the night)
- a physical examination
- blood tests, which may show inflammation.
What tests are there for ankylosing spondylitis?
A blood test can sometimes show if there’s inflammation in the body. You’ll probably have one or more of these tests:
- C-reactive protein (CRP)
- erythrocyte sedimentation rate (ESR)
- plasma viscosity (PV).
These all test for inflammation, so they give similar information. Different laboratories use particular tests. Only 30–40% of people with ankylosing spondylitis have inflammation that can be picked up in a blood test, so in many cases these blood tests will be normal.
Another blood test can confirm whether you have the HLA-B27 gene. Most people with ankylosing spondylitis test positive for HLA-B27, but so do some people who don’t have the condition. A positive test may point to AS but it won’t confirm the diagnosis.
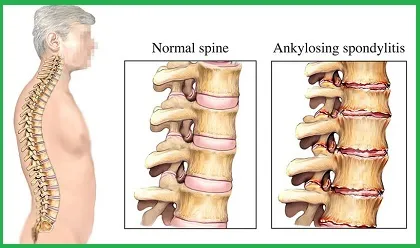
X-rays sometimes help to confirm the diagnosis, though they generally don’t show anything unusual in the early stages. As the condition progresses new bone develops between the vertebrae, which will be visible in x-ray images. However, it may be several years before these signs show up in x-rays. Magnetic resonance imaging (MRI) scans may show changes in the spine or sacroiliac joints at an earlier stage of the disease.
You may need further tests, especially in the early stages. MRI scans may show the typical changes in your spine and at the sacroiliac joints at an earlier stage of the disease and before changes can be identified on x-rays.
Acupuncture treatment for ankylosing spondylitis (AS)
Acupuncture can’t cure the conditions, but researches done in China show needles applied to the Governing Vessel (Du Meridian) combined with moxibustion And Tui Na therapy significantly reduce pain levels and improve the mobility in ankylosing spondylitis patients.
An experienced acupuncturist can also put together a programme of exercises that increase your muscle strength and help you maintain mobility in your spine and other joints. It’s especially important to exercise your back and neck to avoid them stiffening in a bent position.
An acupuncturist will advise you on how to maintain good posture and may also be able to offer you hydrotherapy, which involves special exercises in a warm-water pool. Many people with AS find this therapy helpful and continue their programme at their local leisure pool or with a professional personal trainer.